AI Integration and Its Impact on Clinical Labor
Employing more than 22 million workers and accounting for nearly 20% of annual U.S. GDP, healthcare is a ubiquitous part of American life. There were more than 1 billion office-based doctor’s visits in the U.S. in 2019, or more than 3.2 visits a person, according to the Centers for Disease Control and Prevention.
During each visit, healthcare professionals create, update and archive patient records. These records are vital to ensure continuity and quality of care for patients and serve as primary resources for clinicians and healthcare researchers. And, with more than a billion written up every year, dealing with patient health records is a time-intensive, omnipresent chore for healthcare professionals.
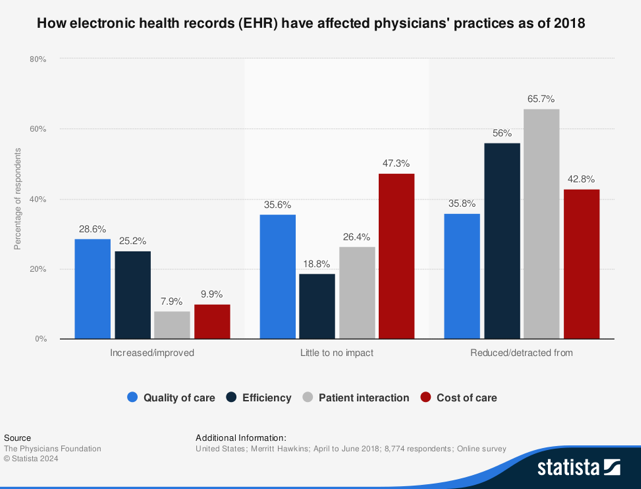
Only recently has the rising digital tide subsumed U.S. health records. From 2011 to 2021, the prevalence of electronic health records, or EHRs, in American hospitals increased from 28% to 96%, according to HealthIT.gov. The EHR revolution has significantly transformed healthcare work and information flows. Digital records enhance accessibility to patients’ medical histories and improve the efficacy of treatment plans, while secure messaging platforms facilitate better communication between physicians and patients. EHRs offer numerous advantages over paper-based records, including coordination between healthcare providers and clinics to increase safety when prescribing medications. And despite concerns about privacy, the move to digitization has generally improved provider-patient interactions and patient data security.1
Yet EHR adoption also has its downsides. Digital information systems have increased administrative burdens on doctors, physician’s assistants, nurses and other healthcare workers, as those using the new electronic interfaces now dedicate greater time and energy to data entry and documentation than ever before. With only so many hours in a shift, time going to administrative tasks is time taken from direct patient care. The additional computer work also means added stress for physicians, increasing clinician fatigue. In a 2018 study of 500 U.S. physicians, 71% reported that EHRs contribute significantly to physician burnout.2
The Promises of AI Integration
This technological challenge has a promising solution: generative AI. Using algorithms trained on open-source information, this technology can produce text, images or audio, and it shows great potential to improve efficiency, reduce burnout and optimize EHR systems in healthcare settings. Major EHR vendors and several health systems have already begun integrating generative AI tools into their platforms. Proponents argue that AI-integrated EHR systems offer clear benefits, enhancing clinic workflow, physician morale and patient care.3 Many hospital administrators are optimistic about the early results. Gary Fritz, chief of applications at Stanford Health Care, highlighted these benefits, saying, “An hour saved … can help rebalance a provider’s too-often overburdened day and cognitive load.”4
One study found that physicians dedicate, on average, more than five hours a day to administering EHRs and more than an hour to EHRs after the workday has ended.5 Generative AI can significantly reduce this documentation burden by automatically generating clinical notes from recorded patient-provider appointments. Physicians would then only need to edit and review the notes to ensure all necessary information is documented. A survey conducted last year by Stanford Health revealed that 78% of physicians reported faster clinical notetaking thanks to a generative AI tool integrated into its Epic EHR system.6 Epic also reported that one provider’s EHR system with AI integration saved 5.5 hours a week, while another provider experienced a 76% reduction in after-hours work.7
Electronic communication between providers and patients is another administrative burden on physicians and health workers that AI technologies can help lift. The COVID-19 pandemic led to a surge in telemedicine, with the number of electronic messages sent by patients soaring to 157% of the pre-pandemic average, and this elevated volume has persisted.8 EHR companies have integrated AI to automate certain tasks such as drafting responses to patients’ messages and suggesting medical codes, saving healthcare workers precious time. The Mayo Clinic has used OpenAI’s large language model, GPT, to automatically generate responses to patients’ messages, finding that this change could save its clinical workers 1,500 hours every month.9
Improved Information Synthesis Leads to Better Care
The potential of artificial intelligence for synthesizing information from EHRs is nearly limitless. Beyond simple regurgitation, generative AI models can analyze EHR data to enhance diagnostics and develop personalized treatment strategies, considering each patient’s unique medical history, genetic makeup and past treatment responses. This type of AI application could improve diagnosis accuracy and treatment effectiveness while minimizing adverse effects. Health systems such as Tufts Medicine, University of Missouri Healthcare and the University of California, Irvine, have integrated AI applications into their operations to provide better, more personalized care to patients.10
These positive outcomes depend on well-trained AI systems designed to minimize bias. If AI algorithms use nonrepresentative training data, they could produce inaccurate reports and unreliable treatment plans. Bias in AI related to EHRs could lead to missing data, sample size underestimation, and misclassification errors.11 It is therefore essential that AI programs incorporate diverse training data, bias detection, transparent code and a strict adherence to official guidelines to mitigate these issues.
Creating Cost Savings
From an institutional healthcare perspective, implementing AI integration with EHRs is a no-brainer, if only for its cost-savings potential. A recent study found that wider adoption of AI could lead to savings of 5% to 10% in total U.S. healthcare spending, or $200 billion to $360 billion annually.12 A separate industry survey found that healthcare organizations reaped a full return on their AI investments within 14 months, on average, and generated $3.20 for every $1 invested in AI.13 These financial benefits come from efficiency gains, as AI integration allows providers to take in more patients with less labor input.
Potential Downsides Require Consideration
The realized and future advantages of integrating AI into EHRs are clear, yet there are also potential disadvantages that should be considered. Reducing administrative burdens allows physicians more time to see more patients, yet it may not be ideal for overworked clinicians to trade less administrative work for more clinical work. By increasing the case burden for physicians, AI-created shift efficiencies could compromise quality of care. AI integration therefore means that healthcare administrators must find a new, optimal balance between maximizing the volume and the quality of care.
All technological change meets resistance, mostly from those tasked with adoption, and AI integration is no different. As providers have implemented AI integration with EHRs, many physicians have expressed concerns about adopting the new interfaces and workflows. This reservation among healthcare workers is understandable considering the added burdens that digitizing health records has already caused. To address fears and facilitate adoption, healthcare institutions will need to carry out workforce training programs that include collaborative efforts between care professionals and technology developers as well as open communication regarding the benefits of incorporating AI into EHRs.
Benefits Will Be Worth the Growing Pains
As new AI tools are adopted across sectors seemingly every day, implementation in healthcare environments warrants increased due diligence. Historically, regulatory entities like the Food and Drug Administration have determined which products were safe to enter a hospital and be used on a patient, and yet regulatory and policy structures may struggle to keep pace in an era of rapid innovation. This challenge likely demands new regulatory pathways that specifically examine AI and software-based tools being developed before they are deployed.
As with any technological paradigm shift, there will be successes and failures of early versions, and winners and losers from a workforce perspective, as some jobs are made redundant or unnecessary. Not all AI tools integrated into EHRs will be worth their initial costs, and improvements in patient care and quality scores may not be realized as quickly as administrators would hope. These hurdles should not dissuade the adoption of AI into healthcare settings, because the opportunities AI offers healthcare providers and patients are monumental, and the long-term quality and cost benefits are likely to be well worth the growing pains of new adoption. As refined platforms and tools emerge and clinicians become accustomed to and familiar with AI technologies, the clinical workforce will likely come to appreciate the improved quality of work-life that AI delivers to their job.
1 What Are the Advantages of Electronic Health Records? HealthIT.Gov, n.d. https://www.healthit.gov/faq/what-are-advantages-electronic-health-records
2 Celik, U., Rath, S., Kesavan, S., & Staats, B. R. (2023). Does Physician’s Choice of When to Perform EHR Tasks Influence Total EHR Workload?. Available at SSRN 4323956.
3 Cool Stuff Now: Epic and Generative AI. (2023, October 13). https://www.epic.com/epic/post/cool-stuff-now-epic-and-generative-ai
4 Armitage, H. (2024, March 11). Ambient artificial intelligence technology to assist Stanford Medicine clinicians with taking notes. Stanford Medicine News Center. http://med.stanford.edu/news/all-news/2024/03/ambient-listening-notes.html
5 Celik, U., Rath, S., Kesavan, S., & Staats, B. R. (2023). Does Physician’s Choice of When to Perform EHR Tasks Influence Total EHR Workload? Available at SSRN 4323956.
6 Dahdah, R. (2024, March 11). Microsoft makes the promise of AI in healthcare real through new collaborations with healthcare organizations and partners. The Official Microsoft Blog. https://blogs.microsoft.com/blog/2024/03/11/microsoft-makes-the-promise-of-ai-in-healthcare-real-through-new-collaborations-with-healthcare-organizations-and-partners/#_edn2
7 Siwicki, B. (2023, November 28). How Epic is using AI to change the way EHRs work. Healthcare IT News. https://www.healthcareitnews.com/news/how-epic-using-ai-change-way-ehrs-work
8 Holmgren, A. J., Downing, N. L., Tang, M., Sharp, C., Longhurst, C., & Huckman, R. S. (2022). Assessing the impact of the COVID-19 pandemic on clinician ambulatory electronic health record use. Journal of the American Medical Informatics Association, 29(3), 453-460.
9 Gen AI Saves Nurses Time by Drafting Responses to Patient Messages. (2024, March 4). EpicShare. https://www.epicshare.org/share-and-learn/mayo-ai-message-responses
10 Horowitz, B. T. (2023, February 10). How Technology Integration Supports Precision Medicine. Technology Solutions That Drive Healthcare. https://healthtechmagazine.net/article/2023/02/how-technology-integration-supports-precision-medicine
11 Gianfrancesco MA, Tamang S, Yazdany J, Schmajuk G. Potential Biases in Machine Learning Algorithms Using Electronic Health Record Data. JAMA Intern Med. 2018 Nov 1;178(11):1544-1547. doi: 10.1001/jamainternmed.2018.3763. PMID: 30128552; PMCID: PMC6347576.
12 Sahni, N., Stein, G., Zemmel, R., & Cutler, D. M. (2023). The potential impact of artificial intelligence on healthcare spending (No. w30857). National Bureau of Economic Research.
13 Dahdah, R. (2024, March 11). Microsoft makes the promise of AI in healthcare real through new collaborations with healthcare organizations and partners. The Official Microsoft Blog. https://blogs.microsoft.com/blog/2024/03/11/microsoft-makes-the-promise-of-ai-in-healthcare-real-through-new-collaborations-with-healthcare-organizations-and-partners/#_edn2