Wrangling Herd Immunity for a Return to the Office
Despite the current political drama playing out in Washington, hope remains for a better 2021. The approvals of the Pfizer-BioNTech and Moderna vaccines provide a clear path for an end to the coronavirus pandemic that challenged almost every aspect of our lives in 2020. But a recent resurgence of the virus and increasing rates of infection indicate that a full return to normalcy—including when and how we go back to the office—is still months in the future.
The office will never be the same
Clearly, workers with a choice will be reluctant to return to the office in pre-pandemic fashion until new cases fall substantially and the desired level of herd immunity is achieved. Until then, organizations will likely stagger hours, require employees to wear masks and modify workspaces to facilitate physical distancing. Companies wanting their workers back in the office sooner may have to offer incentives—for example, offering a daily stipend for onsite work.1 But even a safe office or monetary gain may not be sufficient inducement for some employees, including those who rely on public transportation or have personal constraints (e.g., home schooling or childcare) that complicate a return to the office.
In addition, the more permanent shift in working habits that is underway will also influence when and how office work returns. The grand experiment thrust upon the workplace by the pandemic means that, for some businesses, working remotely will be here to stay. According to McKinsey, 80 percent of employees surveyed reported that they enjoy working from home, with about half as many reporting greater productivity than before.2 Research by Morgan Stanley indicates that about 40 percent of U.S. office workers expect to work at least occasionally from home indefinitely.3 What is clear is that COVID-19 has accelerated pre-pandemic trends in the shift toward remote work—with long-run implications for, among other things, the future of city centers and commercial real estate.4
Herd immunity is critical
Regardless of what’s in store for the long term, how will 2021 play out? There certainly won’t be a celebrated “Back to the Office Day,” but we can still make an educated guess as to when conditions will be conducive to allowing a return to work. Although individual circumstances are likely to vary significantly, a reasonable benchmark for a safe work environment could be the often-cited “herd immunity” threshold, where community transmission starts to decline rapidly. Experts disagree on the precise level of immunity needed, but most believe it to be near 70 percent with a range of 60-80 percent commonly cited.5 With this in mind, we have conducted some back-of-the-envelope calculations to see how long it might take the U.S. to reach herd immunity.
Even a basic model for calculating when the threshold might be reached must take several factors into account, including:
The vaccination rate, which includes the speed with which people are vaccinated and the efficacy of the vaccine.
The past infection rate, encompassing the number of people currently immune because of previous infection and a very low reinfection rate.
The ongoing rate of infection, which assumes that people currently infected will be immune after recovery.
The likelihood that someone already immune is vaccinated, which increases as more and more people are infected.
For our calculations, we generate a reasonable “best guess” for each of these inputs and then examine how sensitive our analysis is to varying these assumptions.
So, what’s the answer?
We estimate that, in our base case, the U.S. will reach a 70 percent immunity threshold around the end of May 2021. But this is just the best guess of a highly uncertain analysis.
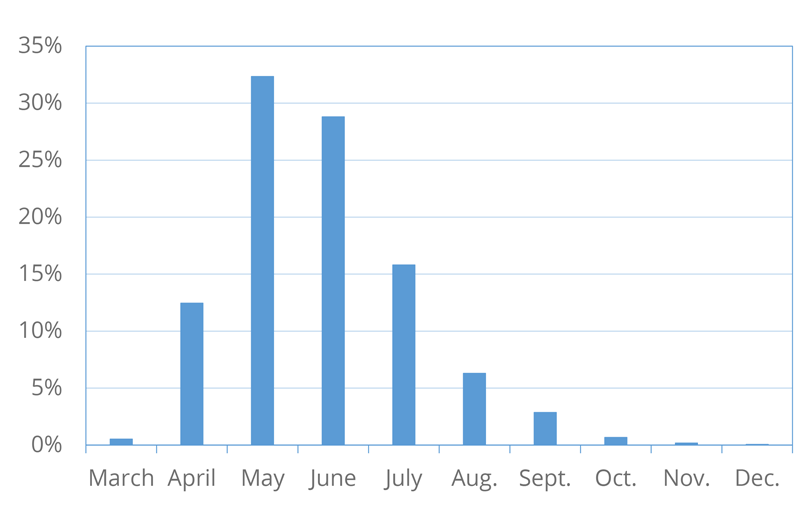
To understand the range of possible outcomes, we conduct a simulation across randomly selected values of our possible inputs.6 The results are shown in Figure 1. Based on our assumptions, we estimate with 90 percent confidence that the U.S. will reach herd immunity sometime between April and the end of September of this year. This implies that our estimates have more downside risk than upside potential: There is almost no chance of herd immunity before April, yet there is a good chance herd immunity will not occur until late summer or early fall.
What factors determine how long it will take?
Our base case assumes a vaccination rate of 30 million people per month. This estimate is based on the expected delivery of 200 million doses of both the Pfizer-BioNtech and Moderna vaccines through July 2021. There is a risk that production or delivery snafus could lower the vaccination rate, so we consider a worst-case scenario of half that, or 15 million people per month.7 On the upside, new vaccines by Johnson & Johnson and AstraZeneca could become available in the coming months, or more of the already approved vaccines could become available in the U.S. if production exceeds expectations. Thus, we assume a best-case scenario of 45 million vaccinations per month.
While a high ongoing infection rate is clearly an undesirable situation, it will speed the time to herd immunity (with all other factors being the same). Reported infections in the U.S. have averaged about 6 million per month recently. In our base case, we assume this rate continues indefinitely. We also consider what would happen if the rate were half or twice this (i.e., 3 million or 12 million per month). At the low end, this would be driven by getting a better handle on current transmission and at the high end, it means a worsening of the pandemic or accounting for unreported cases.
The fact that COVID-19 has already infected millions of people in the U.S. means that the country is part of the way toward herd immunity. The approximately 20 million officially reported cases in the U.S. to date likely represent a small portion of the total number of actual cases, because many people were infected before testing was readily available and infected people often did not seek out a test (e.g., asymptomatic cases). Various statistical models and other inference methods provide a range of estimates for the actual total number of cases in the U.S. Our own analysis suggests it to be currently around 85 million, or 26 percent, of the population, and we use this as our base case.8 Our low-end estimate of 25 million immune individuals assumes that there have been very few undiagnosed cases.9 As a high-end estimate, we assume 115 million currently immune Americans.
Another challenge introduced by the unknown number of people who have been infected is that vaccinations will undoubtedly go to many people who are already immune. Recent research has suggested that prioritizing vaccinations for those who have not been infected could significantly shorten the time it takes to reach herd immunity.10 Although official policies to deprioritize those who have been infected are unlikely, there may be social pressure, correlated policies or behavioral predisposition for those who have been infected to delay or avoid immunization. For example, young healthy adults, who are more likely to have had asymptomatic cases, have low priority unless they are a member of some other high-priority group (e.g., healthcare workers). In addition, many of those who have knowingly been infected may feel it is their civic duty to move themselves to the end of the line. There may also be a correlation between having been infected and an unwillingness to get vaccinated. Individuals who are skeptical of the seriousness of the disease might be more likely to both have avoided precautions (and been infected) and not get vaccinated. We build into our calculation both the drag on herd immunity from vaccinating those who are already immune and a variable that lets us evaluate the effect of prioritizing those who have not already been infected. In our base case, we assume that combined prioritization effects such as those discussed here are 50 percent effective in preventing those already immune from getting vaccinated prior to reaching herd immunity. To gauge the importance of prioritization we consider alternatives with highly effective (90 percent) and highly ineffective (10 percent) prioritization.11
Which factors are most important?
We look at the assumed range of each of the inputs separately to gauge their importance in our estimate. Table 1 summarizes the results.
The exact threshold has a meaningful impact on when we reach herd immunity. If the threshold is 80 percent instead of 70 percent, it will delay reaching the milestone until July, but if it is only 60 percent, the date moves up to April.
| Table 1. Effects of Input Assumptions on When the U.S. Reaches Herd Immunity (Dates are by end of month, 2021) |
|||
|---|---|---|---|
| Input Variable | Worst Case (Slowest) |
Best Case (Fastest) |
Difference (Fastest) |
| Herd Immunity Threshold | July | April | 3 months |
| Ongoing Infection Rate /Month | June | May | 1 month |
| Vaccination Rate /Month | Sept. | April | 5 months |
| Baseline Immunity (already infected/immunized) | July | May | 3 months |
| Prioritization | June | May | 1 month |
By far the largest impact comes from vaccination rates. This is intuitive, given the potential to immunize tens of millions of people each month. Yet even if the vaccination rate were 45 million people per month, it would still take until April to reach herd immunity. Slower production rates or delays in administrating the vaccine (so that only 15 million immunizations are done each month) would postpone the arrival of herd immunity to the end of September.
In contrast, the ongoing infection rate has a small impact on when the U.S. achieves herd immunity. Even if the infection rate in the U.S. were to double, we would be unlikely to reach herd immunity before May. This is consistent with skepticism about accepting higher infection rates in an attempt to reach herd immunity sooner (e.g., as was attempted in Sweden previously).
Our estimate of the current immunity level is moderately important. If many more people are currently immune than in our base case, the herd immunity arrival date would move up by less than a month, but if very few people are currently immune (or lose immunity), the time needed to reach herd immunity is extended by about two months.
In terms of prioritizing vaccination for those who have not been infected, we find limited impact. Even if vaccinations were given to those who have not been previously infected with 90 percent confidence, it would not meaningfully speed the time to herd immunity. A related issue is the ongoing uncertainty as to whether vaccinations prevent transmission by those exposed to the virus, but protected from serious infection or symptoms.
The beginning of the end?
Overall, our assessment of the path to herd immunity is generally positive and roughly in line with statements from some government health officials. For example, at a December event sponsored by Harvard University’s T.H. Chan School of Public Health and the New England Journal of Medicine, National Institute of Allergy and Infectious Diseases Director Anthony Fauci stated that if “…we get 75 percent, 80 percent of the population vaccinated…over the second quarter of 2021, by the time we get to the end of the summer, i.e., the third quarter, we may actually have enough herd immunity protecting our society that as we get to the end of 2021, we can approach very much some degree of normality that is close to where we were before.” Similarly, U.S. Department of Health and Human Services Secretary Alex Azar stated that the recent vaccine procurement deal with Pfizer “…can give Americans even greater confidence we will have enough supply to vaccinate all Americans who want it by the second quarter of 2021.”
But there are downside risks identified by our analysis, as well as risks we did not consider explicitly. Most importantly, our analysis assumes that the majority of people who are currently exposed are willing to get vaccinated. Some recent surveys suggest this may not be the case.12 And being willing is not enough—people must actually follow through and get vaccinated, which currently means getting two shots away from home. It is uncertain how compliant the population will be. In addition, our analysis assumes that the vaccines will remain highly effective in the general population and the virus will not mutate in a way that reduces vaccine efficacy.
Finally, there is a broader range of issues that figure into the U.S. workforce’s return to work away from home. It is tempting to say that as soon as someone is vaccinated, all is clear for them to return. However, even a 95 percent vaccine efficacy rate leaves one in 20 people susceptible to infection. Consequently, some employees will not feel comfortable returning to the office until new infection rates are very low—and “very low” is subjective and dependent on the individual. Companies and managers may hesitate to compel workers to return to the office if they remain sufficiently productive from home.
Additionally, there are growing concerns about cross-border issues, vaccine nationalism and hoarding. How will this affect business travel, which has been almost completely disrupted during the pandemic? How should global businesses think about vaccine coverage when other parts of the world where they operate may face more limited access or be effectively shut out in 2021? For many, returning to work is necessarily global, and part of U.S. labor market resilience depends on whether we allow incoming travel, both business and tourist. Consequently, it may be that, even with herd immunity and a rapidly declining infection rate, many workers will remain remote.
Although the possibility of reaching herd immunity in the U.S. in 2021 brings a much-anticipated light to the end of the pandemic tunnel, it’s clear that the days of sweatpants and bunny slippers as office attire are not over yet—and for some, perhaps may never be.
2 McKinsey & Company, “Reimagining the office and work life after Covid-19”, June 2020.
3 Morgan Stanley Research, “How ‘work from home’ may work for investors”, July 2020.
4 See Davis, Ghent, and Gregory (2020).
5 See Fox et al. (2020). In a December Axios interview, NIAID director Anthony Fauci cited 75-80% of the population as a threshold for herd immunity.
6 Specifically, we simulate the number of months until a random threshold between 60-80 percent immunity is exceeded using a triangular distribution for each of the inputs. The distributions are defined by the base case as the peak value and minimum and maximum values as discussed subsequently. We thank Professor John Butler of the University of Texas Austin McCombs School of Business for generating the simulation results.
7 This is the rate for the complete course, i.e., two shots for both of the currently approved vaccines.
8 See Brown, Ghysels, Yi (2020) which estimates values of 75 million and 94 million through the end of November 2020 based on a Markov model of undetected cases. Other similar estimates are provided by Friedman et al. (2020), Gu (2020), and Reese (2020). The CDC estimates 91 million total infections in the U.S. as of December 11, 2020.
9 Note that this is below levels estimated from seroprevalence surveys and so implicitly assumes reinfection is possible for some individuals. See, for example, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2773576
10 See Bubar et al. (2020).
11 These values can be thought of as determining the probability that an already immune person gets vaccinated and interacts with the current prevalence of immunity in the general population to determine the drag on overall vaccination efficiency.
12 See Hamel et al. (2020) which reports that 27 percent of Americans remain vaccine hesitant with higher rates of vaccine hesitancy among certain groups include those ages 30-49 (39 percent), rural residents (35 percent) and Black adults (35 percent).

