A Shot in the Arm: How COVID-19 Could Transform Healthcare
7 Forces Reshaping the Economy
In this seven-part series of Kenan Insights, we offer a current and in-depth analysis of the findings in our latest report, which explores the economic challenges and opportunities facing our nation amid and beyond both the election and the pandemic. The Kenan Institute of Private Enterprise, in partnership with the North Carolina CEO Leadership Forum, has issued Seven Forces Reshaping the Economy to help decision-makers navigate these critical trends and offer pragmatic solutions to the economic shifts that are defining our new normal. This week, we look at the pandemic’s impact on the healthcare and pharmaceutical industries.
By the time you read this, Election Day in the U.S. will be over. Similar to previous elections, healthcare has remained one of 2020 voters’ top concerns. Although this year’s election was historic for many reasons, one of the main storylines throughout was the largest public health crisis of our time – the global COVID-19 pandemic. As the pandemic continues to cause worrisome health and economic consequences that will need to be addressed in the coming months and years, it also presents opportunities for accelerating innovations in healthcare delivery and pharmaceutical development.
Impacts on Hospitals and Healthcare Providers
Since March 30, COVID-19 has been the third biggest cause of death in the United States, just behind cancer and heart disease, and briefly took the top spot in April.1 Now, as another surge of COVID-19 cases engulfs the country, America’s hospitals and healthcare systems are once again under extreme stress. According to the American Hospital Association, from March-June 2020, hospitals and healthcare systems faced an estimated $202.6 billion in losses, averaging roughly $50.7 billion per month.2 Although Congress was quick to respond with emergency relief funding, it may not be enough to support a system that was already financially strained prior to the outbreak.3 Revenue for the hospital industry as a whole has seen a decline for the past five years. According to IBISWorld, industry revenue has decreased at an annualized rate of 1.5 percent to $945.5 billion over the five years leading up to 2020, including a decline of 18.2 percent in 2020 alone.4 Similarly, pre-pandemic, the Congressional Budget Office projected that 40-50 percent of hospitals could have negative margins by 2025.5
The pandemic has exacerbated these financial constraints. Treating the coronavirus has been costly for many hospitals, as additional labor needs and the rising cost of medical equipment like PPE and ventilators have added to operating costs.6 In addition, early in the pandemic response, the Centers for Medicare and Medicaid Services recommended that “all elective surgeries and nonessential medical, surgical and dental procedures be delayed during the 2019 Novel Coronavirus (COVID-19) outbreak.”7 These elective procedures are important revenue-generating activities for hospitals and other healthcare providers. The Kaiser Family Foundation estimates that by the end of the year, total hospital admissions will be 10.5 percent below predicted volume for the entire year, mainly due to loss of non-emergency procedures.8 These admissions losses will have serious implications for hospital revenues, especially for hospitals operating on small margins.
An Unequal Burden
Rural Hospitals Hit Hard
As the pandemic spreads outside of urban centers and into more rural parts of the U.S., rural hospitals may fall victim to the added burden of dealing with the virus. Rural hospitals have lower per capita capacity, especially with respect to ICU beds, compared to their urban counterparts. Additionally, residents in rural areas are, on average, older and less healthy, increasing the likelihood of the need for intensive care for COVID-19 complications.9 Rural hospitals are also at higher risk of closure. Going into the pandemic, many were extremely financially constrained, with most, on average, having less than a month’s worth of cash on hand.10
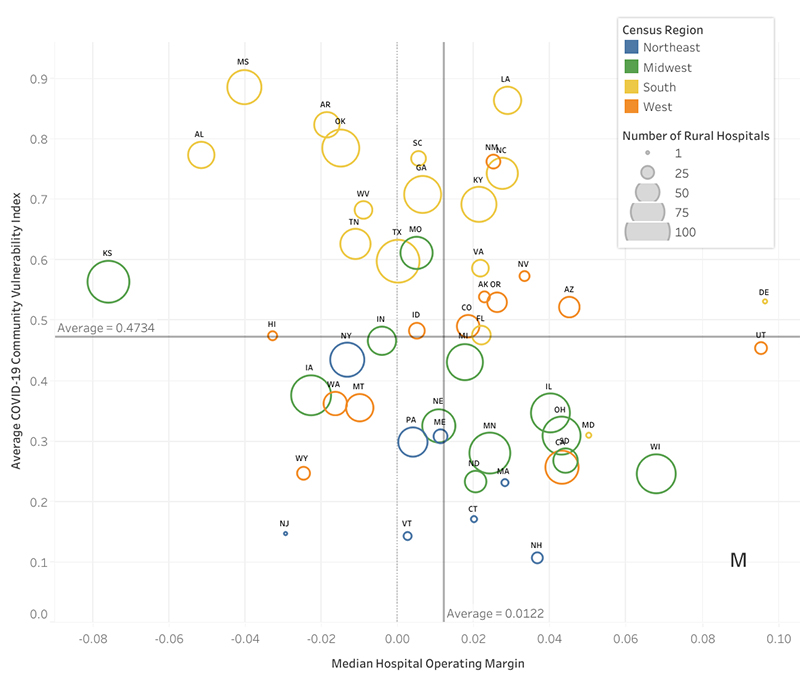
Source: The Cecil G. Sheps Center for Health Services Research11
Addressing Long-Standing Health Disparities for People of Color
Another important need and opportunity is addressing health disparities among people of color. Due to inequities in the U.S. healthcare system, people of color have been disproportionately affected by COVID-19. Infection rates and deaths among people of color are 2.5 times and 1.7 times higher than white people, respectively.12 Black and Native American communities have been particularly hard hit. People of color are facing poorer outcomes due to long-standing discriminatory practices within healthcare systems, limited healthcare access and other societal and economic factors.13 Even prior to the pandemic, research showed systemic racial differences in the quality of care provided to people of color compared to whites, leading to poorer health outcomes.14 The pandemic has amplified these differences.
Opportunities for Innovation in Healthcare and Life Sciences
Although the pandemic has had, and will continue to have, serious consequences for the U.S. healthcare system, it also has presented some unique opportunities to innovate within the healthcare and life sciences spaces. These opportunities include increased efficiencies in public-private partnerships for drug development and distribution, added investment in and acceleration of biopharmaceutical research and production, and further advancements in the use of technology in healthcare delivery.
Public-Private Partnership Necessary to Address Pandemics
The COVID-19 vaccine will likely be developed in record time, putting the capabilities of well-funded scientific endeavors on display and highlighting the importance of public-private partnerships. In the U.S., the federal government is assuming most of the financial risk and lowering the barriers to market entry for vaccine developers. In what is pointedly named “Operation Warp Speed,” the Department of Health and Human Services (DHHS) and Department of Defense (DoD) are overseeing vaccine development and distribution with private sector drug companies.15 As the race for a vaccine continues worldwide, its development and distribution will undoubtedly test global ingenuity as well as require governments to work closely with private sector vaccine developers to quickly respond to both the current and future pandemics.
Biopharmaceutical Research and Production
One of the bright spots in the healthcare industry, and an area for long-term growth and job creation, is biopharmaceutical research and production. Domestic research and production will expand with the willingness to address other risks and the desire to onshore pharmaceutical production capacity and the related supply chain.16 In addition, COVID-19 is highlighting the importance of vaccines — an area that has seen modest growth in recent years. According to BCC Research, in the next five years the global vaccine market is expected to grow at a moderate compound annual growth rate (CAGR) of 6.3 percent. The primary driver of recent growth is an increasing interest by governments in various parts of the world, who assume some of the financial risks, and who have been spurred by outbreaks of major diseases such as Ebola, the Zika virus, chikungunya, avian influenza, the H1N1 virus and COVID-19.17 Conversely, a reversal or refinement of interest in these diseases by governments could change the prospects for economic growth.
| Global Market for Human Vaccines, by Type, through 2025 | |||
|---|---|---|---|
| Type | 2020 | 2025 | CAGR% 2020-2025 |
| Conjugate vaccines | 9,908 | 14,654 | 8.1 |
| Inactivated (killed) vaccines | 5,518 | 7,395 | 6.0 |
| Attenuated (live) vaccines | 6,065 | 7,276 | 3.7 |
| Recombinant/recombinant DNA (rDNA) | 4,288 | 6,797 | 9.7 |
| Subunit vaccines | 2,899 | 4,601 | 9.7 |
| Toxoid vaccines | 1,380 | 1,638 | 3.5 |
| Other/combination vaccines | 4,725 | 4,725 | 2.8 |
| Total | 34,785 | 47,797 | 6.6 |
|
Source: BCC Research, CAGR% is compound annual growth rate in percent
|
|||
Healthcare Teleservices
Another significant near-term shift has been the increase in healthcare teleservices, an industry that has seen rapid expansion in the last five years.18 Due to a number of factors exacerbated by the pandemic, telehealth industry revenue is expected to grow at an annualized rate of 8.3 percent, to roughly $4.8 billion over the next five years.19 Its growth can be attributed to rising healthcare costs, medical professional shortages and an increased demand for medical care for an aging population. Since March 2020, many healthcare providers have replaced traditional appointments with telehealth visits because of stay-at-home orders and infection risks. Growing acceptance of such technologies will lead to long-term opportunities, which will result in new products for healthcare status and compliance monitoring, as well as for mental health services. There has been an immediate and substantial shift toward greater acceptance of remote expertise, but the likelihood of a more permanent move to telehealth/virtual visits is uncertain. While payers have shifted in the current environment to meet the need, hospitals have started marketing and pushing patients to come back to traditional care settings. Hospitals and doctors do not make as much money using telehealth, and with their current financial circumstances, they will likely resist permanent changes.20
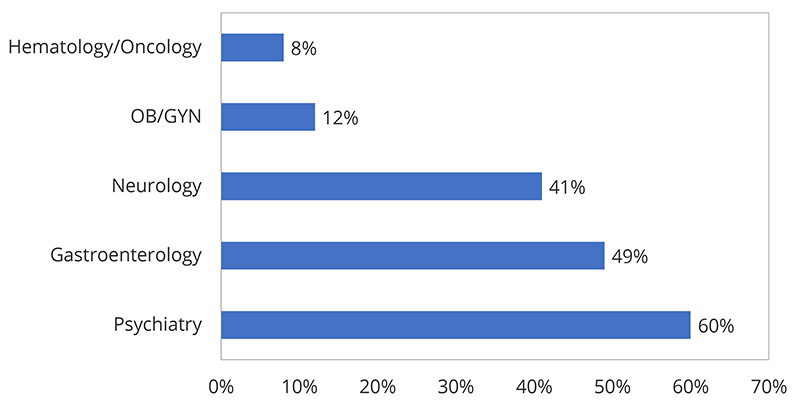
Source: U.S. Department of Health and Human Services21
As health officials warn of the potential for a continued rise in COVID-19 cases through the winter, it will be critical for policymakers, healthcare providers, and private sector vaccine developers to work together to mitigate ongoing risks, especially to vulnerable populations, and to design an equitable and efficient vaccine distribution plan once a vaccine is available. Additionally, it will be important for the healthcare sector to embrace the innovations developed out of necessity during the pandemic, in order to improve care and health outcomes for all going forward.
1 Zhou, Y. & Stix, G. (2020, October 8). COVID-19 is Now the Third Leading Cause of Death in the U.S. Scientific American. Retrieved from https://www.scientificamerican.com/article/covid-19-is-now-the-third-leading-cause-of-death-in-the-u-s1/
2 American Hospital Association. (2020, May). Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19. Retrieved from https://www.aha.org/guidesreports/2020-05-05-hospitals-and-health-systems-face-unprecedented-financial-pressures-due#:~:text=COVID%2D19%20increased%20the%20demand,the%20beginning%20of%20the%20pandemic
3 Hayford, T., Nelson, L., & Diorio, A. (2016). Projecting Hospitals’ Profit Margins Under Several Illustrative Scenarios (Congressional Budget Office Working Paper 2016-04). Retrieved from the Congressional Budget Office website: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/workingpaper/51919-Hospital-Margins_WP.pdf
4 Curran, J. (2020, July). Hospitals in the US (IBISWORLD Industry Report 62211). Retrieved from IBISWorld database.
5 Hayford, T., Nelson, L., & Diorio, A. (2016). Projecting Hospitals’ Profit Margins Under Several Illustrative Scenarios (Congressional Budget Office Working Paper 2016-04). Retrieved from the Congressional Budget Office website: https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/workingpaper/51919-Hospital-Margins_WP.pdf
6 Curran, J. (2020, July). Hospitals in the US (IBISWORLD Industry Report 62211). Retrieved from IBISWorld database.
7 Centers for Medicare & Medicaid Services (2020, March 18). CMS Release Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. Retrieved from https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf
8 Heist, T, Schwartz, K. & Butler, S. (2020, October 19). Trends in Overall and Non-Covid-19 Hospital Admissions. Kaiser Family Foundation. Retrieved from https://www.kff.org/health-costs/issue-brief/trends-in-overall-and-non-covid-19-hospital-admissions/
9 Orgera, K., McDermott, D., Rae, M., Claxton, G., Koma, W, & Cox, C. (2020, April 22). Urban and rural differences in coronavirus pandemic preparedness. Peterson-FF. Retrieved from https://www.healthsystemtracker.org/brief/urban-and-rural-differences-in-coronavirus-pandemic-preparedness/
10 The Cecil G. Sheps Center for Health Services Research. (2020). Rural COVID Research and Figures. Retrieved from https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-covid-research-and-figures/
11 The Cecil G. Sheps Center for Health Services Research. (n.d.) .State Rural Hospital and Community COVID-19 Vulnerability. Retrieved from https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-covid-research-and-figures/rural-hospital-and-community-covid-19-vulnerability/
12 What Still Needs Improvement [Blog Post]. The COVID Tracking Project. Retrieved from https://covidtracking.com/blog/covid-19-race-and-ethnicity-data-whats-changed-and-what-still-needs
13 Centers for Disease Control and Prevention. (2020, July 24)Health Equity Considerations and Racial and Ethnic Minority Groups. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
14 Artiga, S., Orgera, K., & Pham, O. (2020, March 4). Disparities in Health and Health Care: Five Key Questions and Answers. KFF. Retrieved from https://www.kff.org/disparities-policy/issue-brief/disparities-in-health-and-health-care-five-key-questions-and-answers/
15 Lopez, C.T. (2020, June 16). Operation Warp Speed Accelerates COVID-19 Vaccine Development. U.S. Department of Defense. Retrieved from https://www.defense.gov/Explore/News/Article/Article/2222284/operation-warp-speed-accelerates-covid-19-vaccine-development/
16 For example, Kodak recently announced the formation of a new division focused on producing active pharmaceutical ingredients.
17 BCC Research. (2020, September). Global Markets for Vaccine Technologies (BCC Research Report PHM014H). Retrieved from BCC Research Database.
18 Curran, J. (2020, August). Telehealth Services in the U.S. (IBIS World Industry Report OD5775) Retrieved from IBISWorld database.
19 Ibid.
20 Tozzi, J. (2020, June 4). Hospitals Emptied Out by Pandemic Push for Patients to Return. Bloomberg Law. Retrieved from https://news.bloomberglaw.com/coronavirus/hospitals-emptied-out-by-pandemic-push-for-patients-to-return
21 Assistant Secretary for Planning and Evaluation, Health and Human Services (2020). Medicare Beneficiary Use of Telehealth Visits: Early Data from the Start of the COVID-19 Pandemic. Retrieved from: https://aspe.hhs.gov/system/files/pdf/263866/HP_IssueBrief_MedicareTelehealth_final7.29.20.pdf



